Bacteria normally found in the mouth could play a direct role in triggering a heart attack, a new study has found.
In an examination of the arterial plaques collected from more than 200 patients with coronary artery disease, a team of scientists led by Tampere University in Finland found a surprisingly high percentage contained oral bacteria.
“Bacterial involvement in coronary artery disease has long been suspected, but direct and convincing evidence has been lacking,” explains Tampere physician Pekka Karhunen. “Our study demonstrated the presence of genetic material – DNA – from several oral bacteria inside atherosclerotic plaques.”
Related: Poor Oral Hygiene Could Be Taking a Toll on Your Heart, Expert Says
Over the past few decades, a growing body of evidence has established a connection between oral health and cardiovascular health. The two often go hand-in-hand, prompting Karhunen and his colleagues to seek biomarkers that might explain the link.
The focus of their study was one of the main drivers of heart attack: atherosclerosis. This is the buildup of plaque in the coronary arteries, consisting of fat, cholesterol, calcium, and other substances on the artery walls. It narrows the arteries, restricting blood flow, and sometimes even ruptures. This can prevent oxygen from reaching the heart, causing cardiac arrest.
The researchers sampled coronary plaques from 121 patients who had died suddenly, as well as 96 patients who had undergone surgery to remove plaque from their blood vessels.
The team subjected these samples to quantitative polymerase chain reaction analysis, a technique for identifying microbes. They also used immunohistochemistry, which uses antibodies to identify specific toxins, and transcriptomics, which quantifies gene expression levels.
These assays revealed biofilms of several types of oral bacteria, the most common of which belonged to the viridans streptococci group. Oral streptococci were found in 42.1 percent of coronary plaques from the sudden death patients and 42.9 percent of surgery patients.
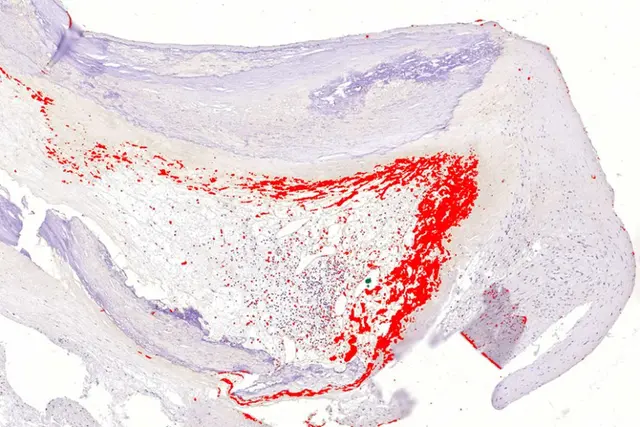
The presence of these bacteria was strongly correlated with severe atherosclerosis, death from heart disease, and death from a heart attack, the researchers found, particularly associated with a ruptured plaque.
The bacterial biofilms tended to be found right at the core of the plaques, out of reach of the body’s immune response. If something else happens to the patient that adds more stress to the body, the biofilm could become inflamed, causing the plaque to rupture, thus triggering a heart attack.
The researchers believe that other bacterial infections, respiratory viruses, poor diet, or the stress hormone norepinephrine could be potential culprits for triggering that inflammation.
Further investigation is needed to narrow down the role of oral bacteria in heart attacks, as well as identify the dangerous exacerbating factors and how the bugs get there in the first place. However, the results strongly suggest that oral health is far more important to heart health than we knew.
“The present results suggest that the change from a stable soft‐core coronary atheroma into a vulnerable rupture‐prone coronary plaque, as well as the development of a symptomatic peripheral artery plaque, may be contributed to by a chronic bacterial infection in the form of a dormant biofilm that colonizes the lipid core and wall of the atheroma and evades immune detection,” the researchers write in their paper.
“This finding adds to the current conception of the pathogenesis of myocardial infarction and opens new possibilities for the diagnostics and prevention of the fatal complications of atherosclerosis.”
The research has been published in the Journal of the American Heart Association.
Source link