Oddly, about 20% of the B cells in our bodies are autoreactive. They target antigens belonging to our own tissues — not by design, but due to the random way B-cell diversity comes about: through sloppy replication, apparently engineered by evolution to ensure diversification. Fortunately, these B cells are typically in a dopey state of inertia, and they pretty much leave our tissues alone.
But at times, somnolent autoreactive B cells become activated, take aim at our own tissues and instigate one of the disorders collectively called autoimmunity. Some awakened autoreactive B cells crank out antibodies that bind to proteins and DNA inside the nuclei of our cells. Such activated “antinuclear antibodies” — the hallmark of lupus — trigger damage to tissues randomly distributed throughout the body, because virtually all our body’s cells have nuclei.
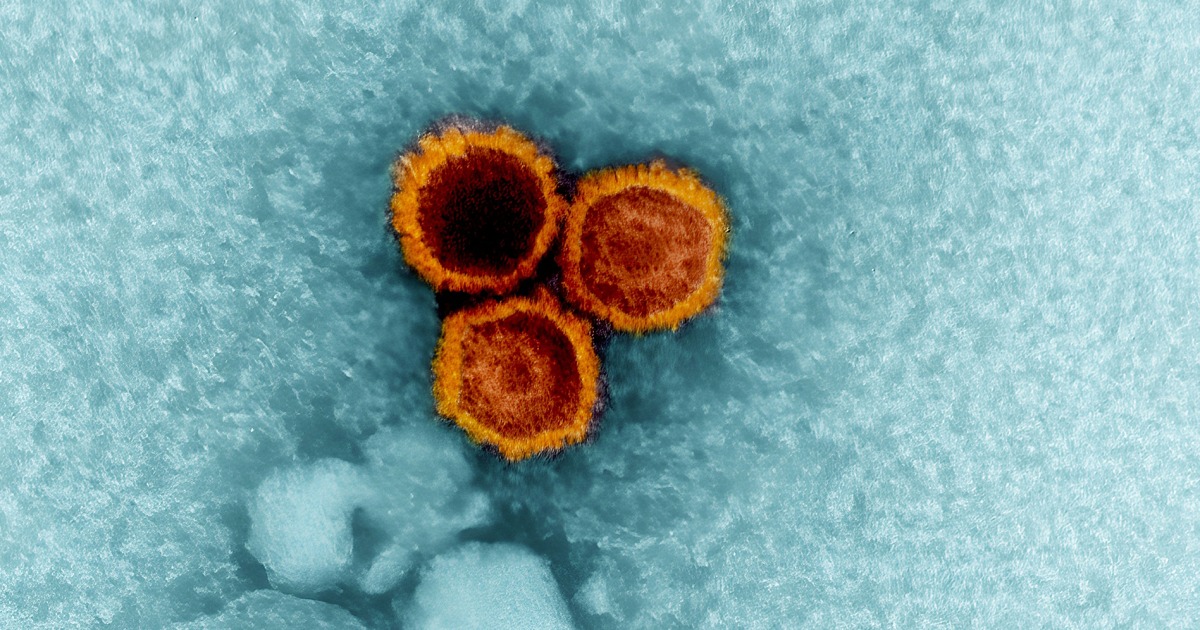
The vast majority of EBV-infected people (most of us, that is) have no idea they’re still sheltering a virus and never get lupus. But essentially everyone with lupus is EBV-infected, studies have shown. An EBV-lupus connection has been long suspected but never nailed down until now.
The antinuclear B cell gets ornery
Although latent EBV is ubiquitous in the sense that almost everybody carries it, it resides in only a tiny fraction of any given person’s B cells. As a result, until the new study, it was virtually impossible for existing methods to identify infected B cells and distinguish them from uninfected ones. But Robinson and his colleagues developed an extremely high-precision sequencing system that enabled them to do this. They found that fewer than 1 in 10,000 of a typical EBV-infected but otherwise healthy individual’s B cells are hosting a dormant EBV viral genome.
Employing their new EBV-infected-B-cell-identifying technology along with bioinformatics and cell-culture experimentation, the researchers found out how such small numbers of infected cells can cause a powerful immune attack on one’s own tissues. In lupus patients, the fraction of EBV-infected B cells rises to about 1 in 400 — a 25-fold difference.
It’s known that the latent EBV, despite its near-total inactivity, nonetheless occasionally nudges the B cell it’s been snoozing in to produce a single viral protein, EBNA2. The researchers showed that this protein acts as a molecular switch — in geneticists’ language a “transcription factor” — activating a battery of genes in the B cell’s genome that had previously been at rest. At least two of the human genes switched on by EBNA2 are recipes for proteins that are, themselves, transcription factors that turn on a variety of other pro-inflammatory human genes.
The net effect of all these genetic fireworks is that the B cell becomes highly inflammatory: It dons its “professional antigen-presenting cell” uniform and starts stimulating other immune cells (called helper T cells) that happen to share a predilection for targeting cell-nuclear components. These helper T cells enlist multitudes of other antinuclear B cells as well as antinuclear killer T cells, vicious attack dogs of the immune system.
When that militia bulks up, it doesn’t matter whether any of the newly recruited antinuclear B cells are EBV-infected or not. (The vast majority of them aren’t.) If there are enough of them, the result is a bout of lupus.
What comes next?
Robinson said he suspects that this cascade of EBV-generated self-targeting B-cell activation might extend beyond lupus to other autoimmune diseases such as multiple sclerosis, rheumatoid arthritis and Crohn’s disease, where hints of EBV-initiated EBNA2 activity have been observed.
The million-dollar question: If about 95% of us are walking around with latent EBV in our B cells, why do some of us, but not all of us, get autoimmunity? Robinson speculates that perhaps only certain EBV strains spur the transformation of infected B cells into antigen-presenting “driver” cells that broadly activate huge numbers of antinuclear B cells.
Many companies are working on an EBV vaccine, and clinical trials of such a vaccine are underway. But that vaccine would have to be given soon after birth, Robinson noted, as such vaccines are unable to rid an already-infected person of the virus.
Stanford University’s Office of Technology Licensing has filed a provisional patent application on intellectual property associated with the study’s findings and technologies used to obtain them. Robinson, Younis and a third study co-author, Mahesh Pandit, PhD, a postdoctoral scholar in immunology and rheumatology, are named inventors on the application. They are co-founders and stockholders of a company, EBVio Inc., a company exploring an experimental lupus treatment, ultradeep B-cell depletion. This procedure involves total annihilation of all circulating B cells, which are replaced over the following few months by new, EBV-free B cells born continually in the bone marrow. Robinson is also a director of EBVio Inc. and a co-founder and shareholder of Flatiron Bio, LLC.
Researchers from the U.S. Department of Veterans Affairs Medical Center, Cincinnati; the University of Massachusetts School of Medicine; the University of Oklahoma Health Sciences Center; and Rockefeller University contributed to the work.
The study was funded by the National Institutes of Health (grants R01AR078268, R01AI173189-01, PATHO-PH2-SUB_17_23 and R01AI024717), the VA Palo Alto Health Care System, the Lupus Research Alliance and the Brennan Family.
Source link