Fanous, J. et al. Limited impact of Salmonella stress and persisters on antibiotic clearance. Nature https://doi.org/10.1038/s41586-024-08506-6 (2025).
Lopatkin, A. J. et al. Metabolic state more accurately predicts antibiotic lethality than growth rate. Nat. Microbiol. 4, 2109–2117 (2019).
Conlon, B. P. et al. Persister formation in Staphylococcus aureus is associated with ATP depletion. Nat. Microbiol. 1, 16051 (2016).
Manuse, S. et al. Bacterial persisters are a stochastically formed subpopulation of low-energy cells. PLoS Biol. 19, e3001194 (2021).
Ahmad, M., Aduru, S. V., Smith, R. P., Zhao, Z. & Lopatkin, A. J. The role of bacterial metabolism in antimicrobial resistance. Nat. Rev. Microbiol. https://doi.org/10.1038/s41579-025-01155-0 (2025).
Hurdle, J. G., O’Neill, A. J., Chopra, I. & Lee, R. E. Targeting bacterial membrane function: an underexploited mechanism for treating persistent infections. Nat. Rev. Microbiol. 9, 62–75 (2011).
Fisher, R. A., Gollan, B. & Helaine, S. Persistent bacterial infections and persister cells. Nat. Rev. Microbiol. 15, 453–464 (2017).
Stokes, J. M., Lopatkin, A. J., Lobritz, M. A. & Collins, J. J. Bacterial metabolism and antibiotic efficacy. Cell Metab. 30, 251–259 (2019).
Wang, B. et al. Antibacterial diamines targeting bacterial membranes. J. Med. Chem. 59, 3140–3151 (2016).
Uppu, D.S.S.M. et al. Membrane-active macromolecules kill antibiotic-tolerant bacteria and potentiate antibiotics towards Gram-negative bacteria. PLoS One 12, e0183263 (2017).
Kim, W. et al. A new class of synthetic retinoid antibiotics effective against bacterial persisters. Nature 556, 103–107 (2018).
Gray, D. A. et al. Membrane depolarization kills dormant Bacillus subtilis cells by generating a lethal dose of ROS. Nat. Commun. 15, 6877 (2024).
Zheng, E. J. et al. Discovery of antibiotics that selectively kill metabolically dormant bacteria. Cell Chem. Biol. 31, 712–728.e9 (2024).
Ledger, E. V. K., Sabnis, A. & Edwards, A. M. Polymyxin and lipopeptide antibiotics: membrane-targeting drugs of last resort. Microbiology 168, 001136 (2022).
Nang, S. C., Azad, M. A. K., Velkov, T., Zhou, Q. T. & Li, J. Rescuing the last-line polymyxins: achievements and challenges. Pharm. Rev. 73, 679–728 (2021).
Kaye, K. S. et al. Efficacy and safety of sulbactam-durlobactam versus colistin for the treatment of patients with serious infections caused by Acinetobacter baumannii-calcoaceticus complex: a multicentre, randomised, active-controlled, phase 3, non-inferiority clinical trial (ATTACK). Lancet Infect. Dis. 23, 1072–1084 (2023).
Paul, M. et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: an open-label, randomised controlled trial. Lancet Infect. Dis. 18, 391–400 (2018).
Velkov, T., Thompson, P. E., Nation, R. L. & Li, J. Structure-activity relationships of polymyxin antibiotics. J. Med Chem. 53, 1898–1916 (2010).
Pristovsek, P. & Kidric, J. Solution structure of polymyxins B and E and effect of binding to lipopolysaccharide: an NMR and molecular modeling study. J. Med Chem. 42, 4604–4613 (1999).
Buchholz, K. R. et al. Potent activity of polymyxin B is associated with long-lived super-stoichiometric accumulation mediated by weak-affinity binding to lipid A. Nat. Commun. 15, 4733 (2024).
Trimble, M. J., Mlynárčik, P., Kolář, M. & Hancock, R. E. Polymyxin: alternative mechanisms of action and resistance. Cold Spring Harb. Perspect. Med. 6, a025288 (2016).
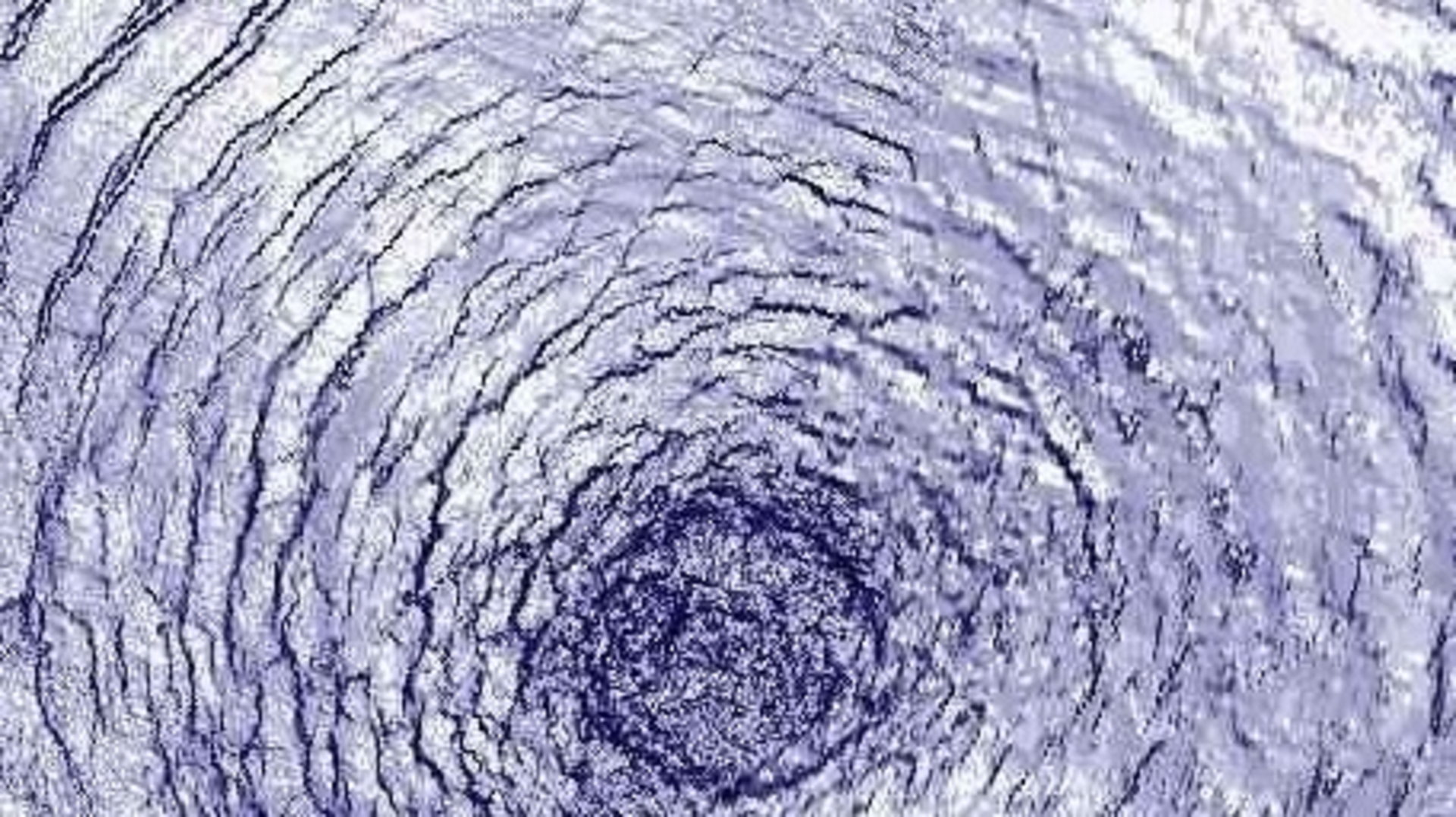
Manioglu, S. et al. Antibiotic polymyxin arranges lipopolysaccharide into crystalline structures to solidify the bacterial membrane. Nat. Commun. 13, 6195 (2022).
Benn, G., Silhavy, T. J., Kleanthous, C. & Hoogenboom, B. W. Antibiotics and hexagonal order in the bacterial outer membrane. Nat. Commun. 14, 4772 (2023).
Manioglu, S. et al. Reply to: Antibiotics and hexagonal order in the bacterial outer membrane. Nat. Commun. 14, 4773 (2023).
Dixon, R. A. & Chopra, I. Polymyxin B and polymyxin B nonapeptide alter cytoplasmic membrane permeability in Escherichia coli. J. Antimicrob. Chemother. 18, 557–563 (1986).
Dixon, R. A. & Chopra, I. Leakage of periplasmic proteins from Escherichia coli mediated by polymyxin B nonapeptide. Antimicrob. Agents Chemother. 29, 781–788 (1986).
Sabnis, A. et al. Colistin kills bacteria by targeting lipopolysaccharide in the cytoplasmic membrane. Elife 10, e65836 (2021).
Humphrey, M. et al. Colistin resistance in Escherichia coli confers protection of the cytoplasmic but not outer membrane from the polymyxin antibiotic. Microbiology 167, 001104 (2021).
Hancock, R. E. & Bell, A. Antibiotic uptake into gram-negative bacteria. Eur. J. Clin. Microbiol. Infect. Dis. 7, 713–720 (1988).
Hancock, R. E. & Chapple, D. S. Peptide antibiotics. Antimicrob. Agents Chemother. 43, 1317–1323 (1999).
Chung, E. S., Wi, Y. M. & Ko, K. S. Variation in formation of persister cells against colistin in Acinetobacter baumannii isolates and its relationship with treatment failure. J. Antimicrob. Chemother. 72, 2133–2135 (2017).
Cui, P. et al. Disruption of membrane by colistin kills uropathogenic Escherichia coli persisters and enhances killing of other antibiotics. Antimicrob. Agents Chemother. 60, 6867–6871 (2016).
McCall, I. C., Shah, N., Govindan, A., Baquero, F. & Levin, B. R. Antibiotic killing of diversely generated populations of nonreplicating bacteria. Antimicrob. Agents Chemother. 63, e02360–18 (2019).
Zavascki, A. P. et al. Pharmacokinetics of intravenous polymyxin B in critically ill patients. Clin. Infect. Dis. 47, 1298–1304 (2008).
Hanafin, P. O. et al. A population pharmacokinetic model of polymyxin B based on prospective clinical data to inform dosing in hospitalized patients. Clin. Microbiol. Infect. 29, 1174–1181 (2023).
Pogue, J. M. et al. Polymyxin susceptibility testing and interpretive breakpoints: recommendations from the United States Committee on Antimicrobial Susceptibility Testing (USCAST). Antimicrob. Agents Chemother. 64, e01495–19 (2020).
Benn, G. et al. Phase separation in the outer membrane of Escherichia coli. Proc. Natl Acad. Sci. USA 118, e2112237118 (2021).
Benn, G. et al. OmpA controls order in the outer membrane and shares the mechanical load. Proc. Natl Acad. Sci. USA 121, e2416426121 (2024).
MacNair, C. R. et al. Overcoming mcr-1 mediated colistin resistance with colistin in combination with other antibiotics. Nat. Commun. 9, 458 (2018).
Heesterbeek, D. A. et al. Bacterial killing by complement requires membrane attack complex formation via surface-bound C5 convertases. EMBO J. 38, e99852 (2019).
Sabnis, A. & Edwards, A. M. Lipopolysaccharide as an antibiotic target. Biochim. Biophys. Acta Mol. Cell Res. 1870, 119507 (2023).
May, J. M. et al. The antibiotic novobiocin binds and activates the ATPase that powers lipopolysaccharide transport. J. Am. Chem. Soc. 139, 17221–17224 (2017).
Mandler, M. D. et al. Novobiocin enhances polymyxin activity by stimulating lipopolysaccharide transport. J. Am. Chem. Soc. 140, 6749–6753 (2018).
Yokota, S. I. et al. Release of large amounts of lipopolysaccharides from Pseudomonas aeruginosa cells reduces their susceptibility to colistin. Int. J. Antimicrob. Agents 51, 888–896 (2018).
Zhang, B. et al. Synthesis of vancomycin fluorescent probes that retain antimicrobial activity, identify Gram-positive bacteria, and detect Gram-negative outer membrane damage. Commun. Biol. 6, 409 (2023).
Ling, Z. et al. Epidemiology of mobile colistin resistance genes mcr-1 to mcr-9. J. Antimicrob. Chemother. 75, 3087–3095 (2020).
Liu et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect. Dis. 16, 161–168 (2016).
Schumann, A. et al. Site-selective modifications by lipid A phosphoethanolamine transferases linked to colistin resistance and bacterial fitness. mSphere 9, e0073124 (2024).
Yang, Q. et al. Balancing mcr-1 expression and bacterial survival is a delicate equilibrium between essential cellular defence mechanisms. Nat. Commun. 8, 2054 (2017).
Weerakoon, D., Petrov, K., Pedebos, C. & Khalid, S. Polymyxin B1 within the E. coli cell envelope: insights from molecular dynamics simulations. Biophys. Rev. 13, 1061–1070 (2021).
Chung, E. S. & Ko, K. S. Eradication of persister cells of Acinetobacter baumannii through combination of colistin and amikacin antibiotics. J. Antimicrob. Chemother. 74, 1277–1283 (2019).
Sahalan, A. Z. & Dixon, R. A. Role of the cell envelope in the antibacterial activities of polymyxin B and polymyxin B nonapeptide against Escherichia coli. Int J. Antimicrob. Agents 31, 224–227 (2008).
Paracini, N., Clifton, L. A., Skoda, M. W. A. & Lakey, J. H. Liquid crystalline bacterial outer membranes are critical for antibiotic susceptibility. Proc. Natl Acad. Sci. USA 115, E7587–E7594 (2018).
Ginez, L. D. et al. Changes in fluidity of the E. coli outer membrane in response to temperature, divalent cations and polymyxin-B show two different mechanisms of membrane fluidity adaptation. FEBS J. 289, 3550–3567 (2022).
McLeod, G. I. & Spector, M. P. Starvation- and stationary-phase-induced resistance to the antimicrobial peptide polymyxin B in Salmonella typhimurium is RpoS (sigma(S)) independent and occurs through both phoP-dependent and -independent pathways. J. Bacteriol. 178, 3683–3688 (1996).
Seo, J., Na, I. Y. & Ko, K. S. Antibiotic efficacy in Escherichia coli and Klebsiella pneumoniae under nutrient limitation and effectiveness of colistin-based antibiotic combinations to eradicate persister cells. Curr. Microbiol. 81, 34 (2023).
Dwyer, D. J., Kohanski, M. A. & Collins, J. J. Role of reactive oxygen species in antibiotic action and resistance. Curr. Opin. Microbiol. 12, 482–489 (2009).
Ma, B. et al. The antimicrobial peptide thanatin disrupts the bacterial outer membrane and inactivates the NDM-1 metallo-β-lactamase. Nat. Commun. 10, 3517 (2019).
Wei, X. et al. Murepavadin induces envelope stress response and enhances the killing efficacies of β-lactam antibiotics by impairing the outer membrane integrity of Pseudomonas aeruginosa. Microbiol. Spectr. 11, e0125723 (2023).
Werneburg, M. et al. Inhibition of lipopolysaccharide transport to the outer membrane in Pseudomonas aeruginosa by peptidomimetic antibiotics. Chembiochem 13, 1767–1775 (2012).
Goode, A., Yeh, V. & Bonev, B. B. Interactions of polymyxin B with lipopolysaccharide-containing membranes. Faraday Discuss. 232, 317–329 (2021).
Sampson, T. R. et al. Rapid killing of Acinetobacter baumannii by polymyxins is mediated by a hydroxyl radical death pathway. Antimicrob. Agents Chemother. 56, 5642–5649 (2012).
Gadar, K. et al. Disrupting iron homeostasis can potentiate colistin activity and overcome colistin resistance mechanisms in Gram-negative bacteria. Commun. Biol. 6, 937 (2023).
Brochmann, R. P. et al. Bactericidal effect of colistin on planktonic Pseudomonas aeruginosa is independent of hydroxyl radical formation. Int. J. Antimicrob. Agents 43, 140–147 (2014).
Kolpen, M. et al. Increased bactericidal activity of colistin on Pseudomonas aeruginosa biofilms in anaerobic conditions. Pathog. Dis. 74, ftv086 (2016).
Koike, M., Iida, K. & Matsuo, T. Electron microscopic studies on mode of action of polymyxin. J. Bacteriol. 97, 448–452 (1969).
Lounatmaa, K., Mäkelä, P. H. & Sarvas, M. Effect of polymyxin on the ultrastructure of the outer membrane of wild-type and polymyxin-resistant strain of Salmonella. J. Bacteriol. 127, 1400–1407 (1976).
Manning, A. J. & Kuehn, M. J. Contribution of bacterial outer membrane vesicles to innate bacterial defense. BMC Microbiol. 11, 258 (2011).
Park, J. et al. A novel decoy strategy for polymyxin resistance in Acinetobacter baumannii. Elife 10, e66988 (2021).
Kulkarni, H. M., Nagaraj, R. & Jagannadham, M. V. Protective role of E. coli outer membrane vesicles against antibiotics. Microbiol. Res. 181, 1–7 (2015).
Sabnis, A., Ledger, E. V. K., Pader, V. & Edwards, A. M. Antibiotic interceptors: creating safe spaces for bacteria. PLoS Pathog. 14, e1006924 (2018).
McBroom, A. J. & Kuehn, M. J. Release of outer membrane vesicles by Gram-negative bacteria is a novel envelope stress response. Mol. Microbiol. 63, 545–558 (2007).
Brand, C., Newton-Foot, M., Grobbelaar, M. & Whitelaw, A. Antibiotic-induced stress responses in Gram-negative bacteria and their role in antibiotic resistance. J. Antimicrob. Chemother. 80, 1165–1184 (2025).
Steenhuis, M., Ten Hagen-Jongman, C. M., van Ulsen, P. & Luirink, J. Stress-based high-throughput screening assays to identify inhibitors of cell envelope biogenesis. Antibiotics 9, 808 (2020).
Audrain, B. et al. Induction of the Cpx envelope stress pathway contributes to Escherichia coli tolerance to antimicrobial peptides. Appl. Environ. Microbiol. 79, 7770–7779 (2013).
Erickson, K.D. & Detweiler, C.S. The Rcs phosphorelay system is specific to enteric pathogens/commensals and activates ydeI, a gene important for persistent Salmonella infection of mice. Mol. Microbiol. 62, 883–894 (2006).
Wang, D., Korban, S. S. & Zhao, Y. The Rcs phosphorelay system is essential for pathogenicity in Erwinia amylovora. Mol. Plant Pathol. 10, 277–290 (2009).
Rojas, E. R. et al. The outer membrane is an essential load-bearing element in Gram-negative bacteria. Nature 559, 617–621 (2018).
Arunmanee, W. et al. Gram-negative trimeric porins have specific LPS binding sites that are essential for porin biogenesis. Proc. Natl Acad. Sci. USA 113, E5034–E5043 (2016).
Peterson, J. H., Yang, L., Gumbart, J. C. & Bernstein, H. D. Conserved lipid-facing basic residues promote the insertion of the porin OmpC into the E. coli outer membrane. mBio 16, e0331924 (2025).
Webby, M. N. et al. Lipids mediate supramolecular outer membrane protein assembly in bacteria. Sci. Adv. 8, eadc9566 (2022).
Davis, K. P. et al. Critical role of growth medium for detecting drug interactions in Gram-negative bacteria that model in vivo responses. mBio 15, e0015924 (2024).
Heithoff, D. M. et al. Re-evaluation of FDA-approved antibiotics with increased diagnostic accuracy for assessment of antimicrobial resistance. Cell Rep. Med. 4, 101023 (2023).
Duong, L. et al. Bactericidal activity of mammalian histones is caused by large membrane pore formation. Cell Rep. 44, 115658 (2025).
Fierer, J. & Finley, F. Lethal effect of complement and lysozyme on polymyxin-treated, serum-resistant Gram-negative bacilli. J. Infect. Dis. 140, 581–589 (1979).
Leeson, M. C., Fujihara, Y. & Morrison, D. C. Evidence for lipopolysaccharide as the predominant proinflammatory mediator in supernatants of antibiotic-treated bacteria. Infect. Immun. 62, 4975–4980 (1994).
Jensen, K. F. The Escherichia coli K-12 “wild types” W3110 and MG1655 have an rph frameshift mutation that leads to pyrimidine starvation due to low pyrE expression levels. J. Bacteriol. 175, 3401–3407 (1993).
Silhavy T. J., Berman M. L. & Enquist L. W. Experiments with Gene Fusions (Cold Spring Harbor Laboratory Press, 1984).
Braun, M. & Silhavy, T. J. Imp/OstA is required for cell envelope biogenesis in Escherichia coli. Mol. Microbiol. 45, 1289–1302 (2002).
Sampson, B. A., Misra, R. & Benson, S. A. Identification and characterization of a new gene of Escherichia coli K-12 involved in outer membrane permeability. Genetics 122, 491–501 (1989).
Mobley, H. L. et al. Pyelonephritogenic Escherichia coli and killing of cultured human renal proximal tubular epithelial cells: role of hemolysin in some strains. Infect. Immun. 58, 1281–1289 (1990).
Dortet, L., Bréchard, L., Poirel, L. & Nordmann, P. Rapid detection of carbapenemase-producing Enterobacteriaceae from blood cultures. Clin. Microbiol Infect. 20, 340–344 (2014).
Wan, Y. et al. Integrated analysis of patient networks and plasmid genomes to investigate a regional, multispecies outbreak of carbapenemase-producing Enterobacterales carrying both blaIMP and mcr-9 genes. J. Infect. Dis. 230, e159–e170 (2024).
Lee, D. G. et al. Genomic analysis reveals that Pseudomonas aeruginosa virulence is combinatorial. Genome Biol. 7, R90 (2006).
Wiegand, I., Hilpert, K. & Hancock, R. E. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat. Protoc. 3, 163–175 (2008).
Odds, F. C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 52, 1 (2003).
Benn, G., Pyne, A. L. B., Ryadnov, M. G. & Hoogenboom, B. W. Imaging live bacteria at the nanoscale: comparison of immobilisation strategies. Analyst 144, 6944–6952 (2019).
Nečas, D. & Klapetek, P. Gwyddion: an open-source software for SPM data analysis. Cent. Eur. J. Phys. 10, 181–188 (2012).
Buttress, J. A. et al. A guide for membrane potential measurements in Gram-negative bacteria using voltage-sensitive dyes. Microbiology https://doi.org/10.1099/mic.0.001227 (2022).
Larrouy-Maumus, G., Clements, A., Filloux, A., McCarthy, R. R. & Mostowy, S. Direct detection of lipid A on intact Gram-negative bacteria by MALDI-TOF mass spectrometry. J. Microbiol. Methods 120, 68–71 (2016).
Source link