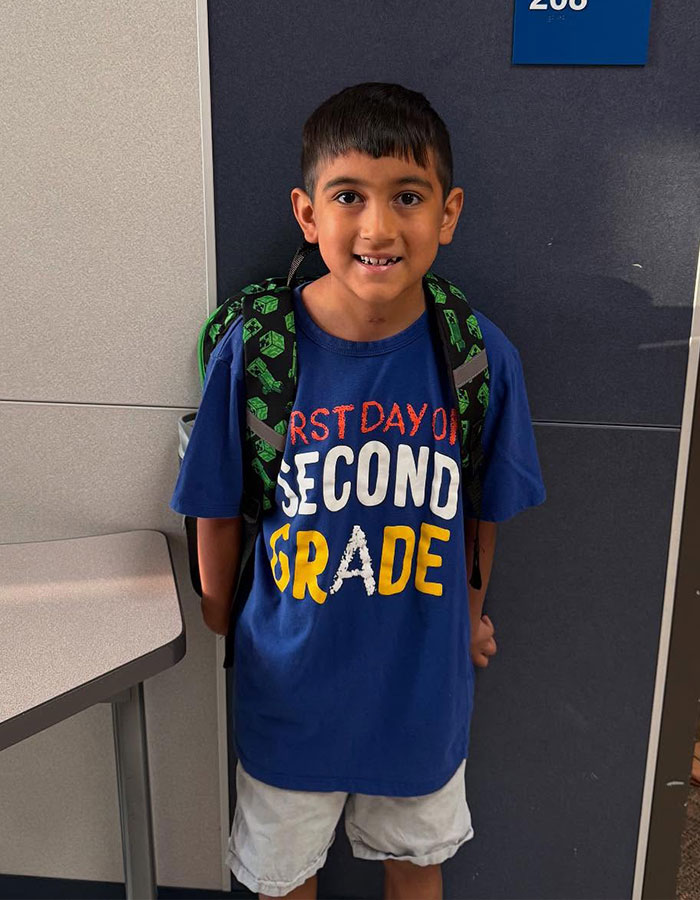
Texas mom Casey Daniel was told her young son Witten had the flu, only for him to become paralyzed hours later—because of a rare brain disorder that makes cells bleed.
The boy, a little league MVP, lost his ability to walk, talk, and even breathe independently in 24 hours.
Doctors then realized that the child had a cavernoma—a mulberry-like cluster of leaking cells near his brain stem.
- Texas mom says son was misdiagnosed with flu hours before paralysis set in.
- MRI later revealed a cavernous malformation near his brain stem, a rare disorder affecting 1 in 2,000.
- Connie Lee, Alliance to Cure CEO, says seizures and face drooping are key warning signs.
The prognosis was dark: Casey heard that due to the condition that affects 1 in every 2,000 people, her boy would likely never walk again.
In another case, a pediatrician thought it was an earache
Image credits: caseyarend
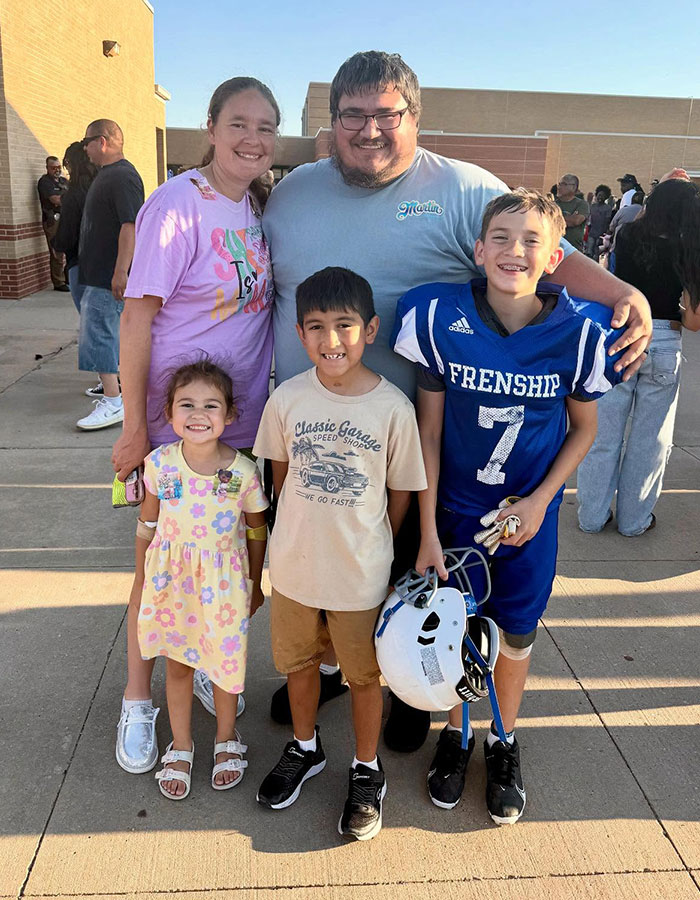
Another person to witness the medical anomaly in their offspring is Connie Lee.
She recalls how her four-month-old daughter struggled to sleep and started becoming progressively more irritable over the course of a week.
Like Daniel’s case, the doctor initially thought the infant was suffering from a minor ailment.
Image credits: caseyarend
The pediatrician observed the child’s raised fontanelle (the soft spot on an infant’s skull), pondered on the probability of an earache, and prescribed amoxicillin.
An MRI showed that Connie Lee’s daughter had multiple tumors on her brain
When Lee returned home, her baby had started projectile vomiting, and thus she could not keep the medication down.
This prompted a call to the doctor, who then scheduled an MRI at a children’s hospital.
Image credits: caseyarend
The resulting imagery would show that Lee’s months-old daughter’s brain had numerous tumors, the largest of which was four centimeters.
“She was in crisis,” Lee recalled. “Had she not had the brain surgery that day, she would not be with us now.”
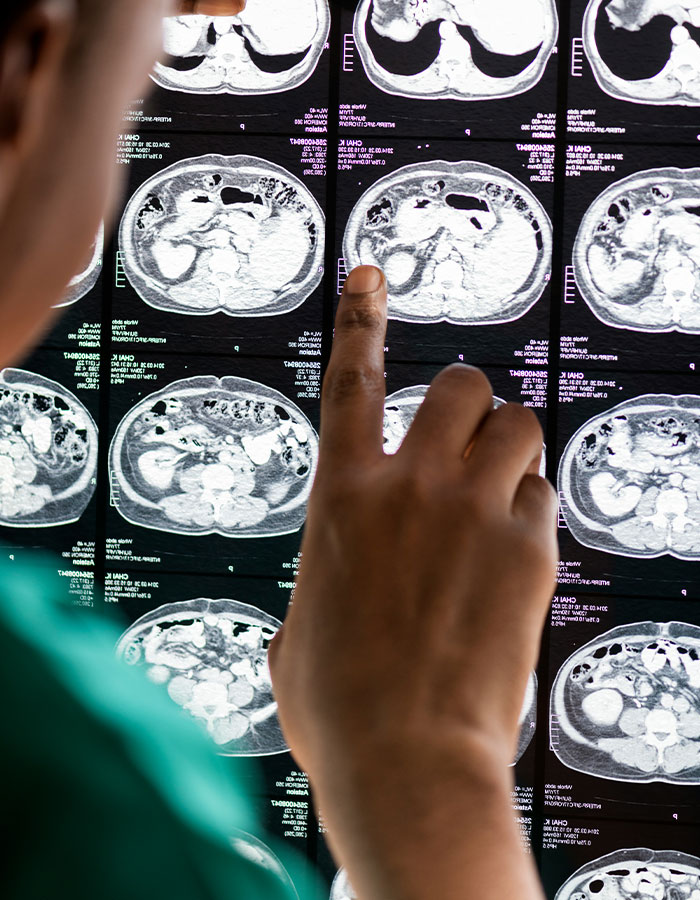
Cavernous Malformations are raspberry-like clumps of leaking brain cells
Connie Lee is also the CEO of the Alliance to Cure Cavernous Malformation, a patient research foundation and advocacy for people with the disorder .
Answering questions for Bored Panda on September 20, she described the condition as “abnormal” and “leaky” blood vessels that look like “a raspberry or mulberry.”
“Blood tends to flow through them pretty slowly because they’re in the capillaries of the brain blood vessels and they can occur anywhere in the brain or in the spinal cord,” she explained.
Seizures are a telling sign of the disorder
Lee goes on to say that the most telling symptoms of cavernous malformation include focal seizures, which affect at least 50 percent of patients.
Image credits: Getty/Unsplash
These events affect an area of the brain triggering failures in speech and vision and involuntary behaviors in the body while the patient is still conscious.
She further notes that the symptoms experienced by the patient “depends on where the cavernous malformations are located,” explaining that they can translate into “abnormal body” movements and “weird smells that no one else around [the patient] can smell.”
“About fifty percent show up with seizures that are focal seizures, meaning the seizures happening in just a small area of the brain,” Lee elaborated.
Another sign of Cavernous Malformation is a drooping face
Image credits: alliancetocure
“Other folks, when they first have a Cavernous Malformation symptom, will have some sort of neurological deficit,” her explanation continued.
“It can be face drooping or vision issues, weaknesses, numbness, tingling in arms and legs.
“Those are not necessarily related to the most severe presentation of CCM (cerebral cavernous malformation), which is hemorrhage.
Lee went on to say Witten Daniel, the little boy who suffered complete paralysis in a matter of hours, fell into the category of CCM patients whose leaking blood vessels become full brain hemorrhages.
Children and infants are more inclined to suffer sudden deteriorations
Image credits: Curated Lifestyle/Getty
Among kids and infants, the condition more often than not goes undetected until the hemorrhage has progressed, and this is because they have difficulty accurately explaining what they are experiencing.
“And so for little kids, when we get to a point where this becomes emergent, where there’s an emergency, what we see are things like vomiting, projectile vomiting, floppiness, so this loss of muscle tone in infants especially.”
“And it can be mistaken for something that’s not as severe. The vomiting can be easily mistaken for flu,” Lee says, as a nod to Daniels’ experience.
Image credits: caseyarend
She explains that although sudden deterioration like Witten’s is rare; it is more common in children.
Upon experiencing symptoms, individuals should see a doctor or go to an emergency room
Responding to the question on what action to take at the onset of these symptoms, Lee says that patients “certainly should take themselves to the emergency room to be checked, and that would include face drooping.”
Image credits: caseyarend
“That can sometimes just be something as simple as Bell’s palsy, which is not a serious condition.
“It often resolves on its own, but it can also be the sign of something more serious. It’s better to be safe.
“The folks who are having focal seizures, that’s not as much of an emergency. You can take that to your regular doctor and then get a referral to neurology for further workup to see if there is some explanation for it.”
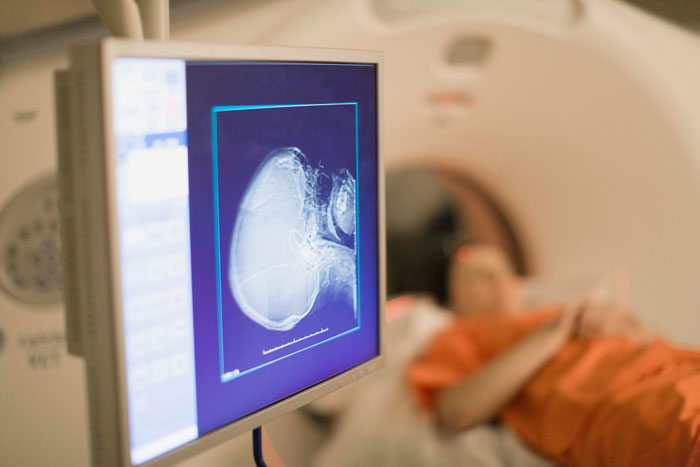
Lee explains that the most certain way to know is through diagnosis, which usually involves a CT scan and then an MRI.
Only two percent of Cavernous Malformation patients pass away
Fortunately, Witten’s sudden deterioration is not the norm, and the suddenness with which debilitates differ from person to person.
And as harrowing and jarring as the effects may be, only two percent of diagnosed cases result in patients passing away eventually.
Image credits: UTHealth Houston
“By and large, everyone else who has a cavernous malformation will either recover, and most people, even those who have brain hemorrhage, if it’s higher in the brain, frequently have good recovery, even almost back to normal, or if it’s in lower parts of the brain, they continue to have disabilities and deficits,” Lee elaborates.
Notably, due to the “higher plasticity” of children’s brains, they have a better chance of making faster and fuller recoveries.
The only way to get a sure diagnosis is with an MRI
Image credits: caseyarend
Lee’s organisation, Alliance to Curenotes Cavernous Malformation is a rare disease.
Be that as it may, MRIs help with diagnosis with treatment options thereafter being available.
“So if there is a referral to MRI, the diagnosis is pretty simple and straightforward. To diagnose it works,” Lee observed.
But getting a doctor to schedule an MRI can be tricky
“So what stands in the way of getting an MRI? Multiple things. First off, the doctor needs to or the health care provider needs to believe you.
“When you’re having neurological symptoms, sometimes they get tossed off as psychiatric symptoms or get attributed to some other physical disease that’s happening.
“And so it may take a while before you actually get to the point where the doctor will say, Oh, there’s something going on in your brain. We should give you an MRI.”
Children and certain “populations” are not favored candidates for MRI’s
“I think particularly there are populations in our country (the US) that don’t get the benefit of the doubt in the same way as others,” Lee observed, “and those folks typically take longer to get a diagnosis.
“A second issue that gets in the way of diagnosis is with kids,” she continued.
“Kids need to be sedated in order to have an MRI. MRI requires you to lie still for twenty five minutes or more, and children just can’t sustain that.
“So the sedation itself is a big deal. It requires time in pre op, in the MRI, and then in a recovery area.”
Witten Daniel is home and well, and planning his return to the baseball field
As a testimony to Lee’s assertions of the low mortality rate surrounding Cavernous Malformation, her daughter and Witten Daniel have made the next best thing to full recoveries.
In Daniel’s case, it was Casey’s refusal to accept her son’s fate.
Following a Google search, she connected with neurosurgeons Dr. Manish Shah and Dr. Jacques Morcos at Houston’s UTHealth.
As a result of this interaction, her son, now seven, is home again, preparing to return to the baseball field, perKCBD.
It appears the internet rallied behind Witten Daniels
Thanks! Check out the results:
Total votes ·