A major Alzheimer’s disease medical group is recommending that specialists may use certain blood tests to help diagnose patients with cognitive impairment in lieu of more complex and invasive tests, a move that could lead more people to get treated for the devastating disease.
The Alzheimer’s Association, in its first clinical guidelines on blood biomarker testing, said Tuesday that tests that have over 90% sensitivity (ability to identify positive results) and 90% specificity (ability to identify negative results) can be used instead of current diagnostic methods like PET scans and cerebrospinal fluid tests.
The group said that tests that have over 90% sensitivity and 75% specificity can be used to triage patients, meaning negative results rule can rule out Alzheimer’s with high probability but positive results should be confirmed with the standard diagnostic methods, given that these blood tests have a higher likelihood of false positives.
The authors stressed that the guidelines should not be considered a substitute for a full clinical evaluation and that they apply only to people who are in the care of specialists and have already been confirmed to have cognitive impairment. The authors also noted that there’s wide variability in the blood tests on the market and that many do not meet the accuracy thresholds.
They did not endorse specific tests, but reviewed dozens that measured biomarkers such as pTau217, the ratio of pTau217 to non-pTau217, and the ratio of Aβ42 to Aβ40. They will post a chart of the various tests and their accuracy in an online portal that will be continually updated, said Rebecca Edelmayer, one of the guidelines’ authors and vice president of scientific engagement at the Alzheimer’s Association.
The approval of new Alzheimer’s drugs in recent years has ignited a race to roll out blood tests as a more convenient and cheaper way for patients to get diagnosed, and so far the Food and Drug Administration has approved one test. But up until now, doctors haven’t had clear guidelines on when to use them.
While the recommendations are expected to be updated over time, even the first stab could lead to more patients getting tested and diagnosed, particularly in rural areas, where access to scans and spinal fluid tests are typically more difficult to access.
“I think this is reasonable. They’ve really thought through this very carefully in terms of making a diagnosis,” said Joseph Quinn, a professor of neurology at Oregon Health & Science University who was not involved in writing the guidelines.
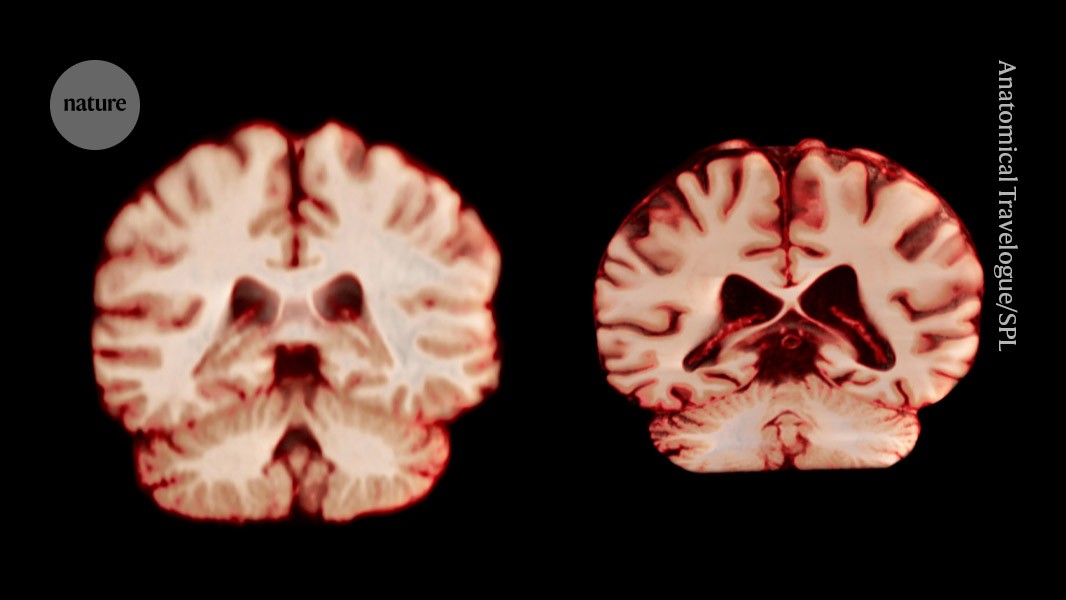
It’s still best for patients who plan to start treatment to receive PET scans first, said Stephen Salloway, a professor of neurology at Brown University who was not involved with the guidelines. New therapies from Eisai, Biogen, and Eli Lilly aim to shrink a plaque in the brain called amyloid that’s thought to be linked to Alzheimer’s, and doctors, if possible, should scan patients not only before treatment but throughout treatment to ensure that the amyloid is shrinking, he said.
The blood tests can detect whether patients are positive or negative for amyloid, but are not reliable measures of how much amyloid is in their brain, said Salloway, who has consulted for drug companies making Alzheimer’s treatments.
The recommendations do not address how to use blood tests in the course of monitoring patients receiving treatment.
Drugmakers have supported the development of blood tests, and Lilly has been trying to make it easier for patients to get diagnosed, recently striking an agreement with a telehealth provider in which it connects patients to a virtual platform so they can get a diagnosis if necessary and get a prescription for treatment.
To make the guidelines, the authors reviewed close to 50 studies. They excluded studies that analyzed populations of people who both did and didn’t have cognitive impairment, since they wanted to focus only on those with cognitive impairment. They only evaluated tests that used a single threshold that determined positive or negative results. And they also rated how certain the evidence was for each test’s accuracy.
The guidelines also serve as a “call to action” for researchers to understand how to conduct studies and publish results in a way for the Alzheimer’s Association to deem the tests as having strong evidence backing them up, said Edelmayer.
Source link