You’d assume that a medicine you can buy without a prescription at any pharmacy, big-box retailer, or grocery store is completely safe, right? But as more research comes out, we’re learning that over-the-counter (OTC) drugs can come with a long list of potentially dangerous side effects. The latest such study shows that two very popular and very common pain meds may be fueling antibiotic resistance.
RELATED: Doctors Warn This Popular Med Is “The Most Dangerous OTC Drug.”
What’s the deal with antibiotic resistance?
As the name suggests, antibiotic resistance occurs when bacteria change and no longer respond to antibiotic medicines, making certain bacterial infections difficult or impossible to treat, as Cleveland Clinic explains. The most common reason for this is the overuse of antibiotics.
According to a 2023 scientific article published in StatPearls, “In 2015, 30 percent of the outpatient antibiotics prescribed were unnecessary, with acute respiratory infections holding the highest unnecessary use of antibiotics at 50 percent.”
More broadly speaking, antimicrobial resistance (AMR) refers to all instances in which bacteria, viruses, fungi, and parasites stop responding to medicines such as antibiotics, antivirals, antifungals, and antiparasitics.
The World Health Organization (WHO) estimates that “bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths.”
RELATED: Doctors Warn These OTC Antacids Can Put Your Heart in Danger.
Scientists are also concerned about antibiotic resistance caused by other types of medications.
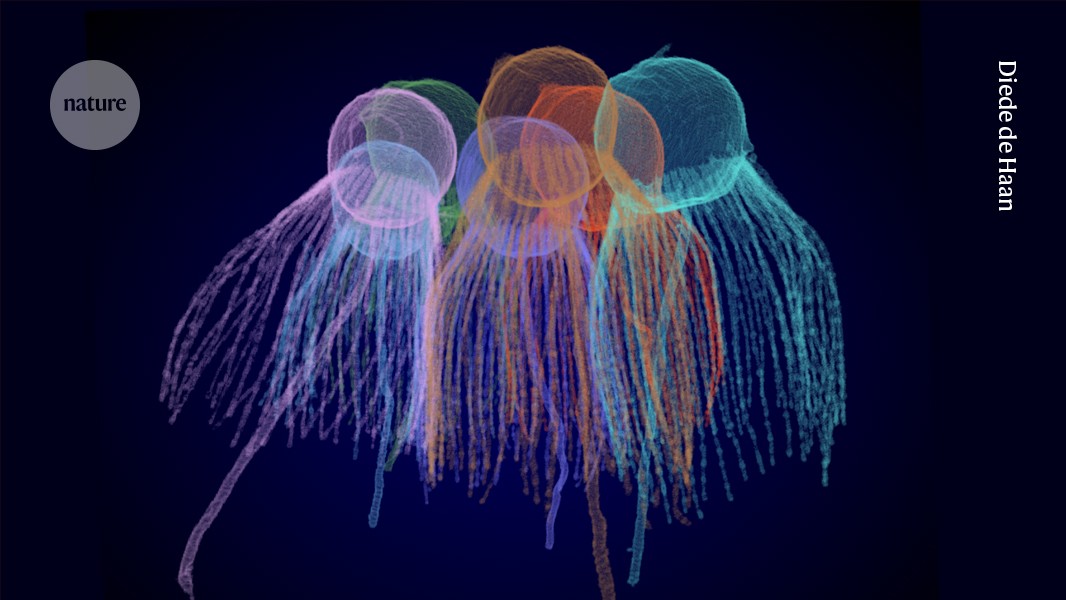
A new study, published in the journal Nature, took a closer look at how non-antibiotic medications may contribute to antimicrobial resistance.
The researchers were especially concerned about the effects in residential aged care facilities, where patients are frequently given both antibiotics and non-antibiotic medications, including those for pain, sleep, and blood pressure.
To arrive at their findings, the scientists from the University of South Australia (UniSA) investigated the effects of nine common non-antibiotic medications on the bacteria Escherichia coli (E. coli):
- Ibuprofen (Advil, an anti-inflammatory pain reliever)
- Diclofenac (Voltaren, an anti-inflammatory pain reliever used to treat arthritis)
- Acetaminophen (Tylenol, a drug to treat pain and fever)
- Furosemide (a blood pressure-lowering drug)
- Metformin (a common diabetes drug)
- Atorvastatin (Lipitor, a cholesterol-lowering drug)
- Tramadol (an opioid pain drug)
- Temazepam (Restoril, a sleeping pill)
- Pseudoephedrine (Sudafed, a decongestant)
E. coli most commonly causes gut (GI tract) infections and urinary tract infections (UTIs). It is treated with the antibiotic ciprofloxacin.
RELATED: Taking Too Much of This Supplement Can Hurt Your Heart, Doctors Warn.
Research shows that Tylenol and Advil can contribute to antibiotic resistance.
Once the researchers had their data, they employed whole-genome sequencing, a technology that determines the exact order of DNA in a human’s genome and can pinpoint genetic mutations.
They found that, of the nine medications, the two common OTC pain meds, Advil and Tylenol, drive antibiotic resistance when used individually and further amplify it when used together.
“When bacteria were exposed to ciprofloxacin alongside ibuprofen and paracetamol, they developed more genetic mutations than with the antibiotic alone, helping them grow faster and become highly resistant,” said lead researcher Rietie Venter, an associate professor at UniSA, in a press release.
“Worryingly, the bacteria were not only resistant to the antibiotic ciprofloxacin, but increased resistance was also observed to multiple other antibiotics from different classes,” she continued. “We also uncovered the genetic mechanisms behind this resistance, with ibuprofen and paracetamol both activating the bacteria’s defences to expel antibiotics and render them less effective.”
Venter explains that the research isn’t advocating for people to stop using Advil and Tylenol, but rather to be more mindful of how much they’re taking or prescribing and with what antibiotics. She and her team are planning further research into drug interactions and antibiotic resistance.
Source link