Imagine a reality where a person who lost the ability to walk due to war, an accident or an injury undergoes surgery and rises to their feet again. A team of Israeli scientists is bringing that dream closer to reality.
The development is led by Prof. Tal Dvir, head of the Sagol Center for Regenerative Biotechnology and the Nanotechnology Center at Tel Aviv University, as well as chief scientist of the biotech company Matricelf. The company was founded in 2019 based on the groundbreaking organ-engineering technology developed by Dvir and his team at the university, under a licensing agreement with Ramot, Tel Aviv University’s technology transfer company.
“The spinal cord is made up of nerve cells that transmit electrical signals from the brain to all parts of the body,” Dvir explained. “The decision is made in the brain, the signal passes down the spinal cord, and neurons activate the muscles. When the cord is torn by trauma — a car accident, a fall or a battlefield injury — the chain is cut. Imagine an electric cable: when two ends don’t touch, the signal doesn’t pass. The cable won’t conduct electricity, and the person cannot pass signals beyond the injury.”
That, he said, is the major difficulty. Spinal cord injury is one of the few traumas in the body with no natural ability to regenerate. “Neurons don’t divide or renew themselves. They’re not like skin cells, which can repair wounds. They’re like heart cells: once damaged, the body cannot restore them,” Dvir said. “The damage stabilizes at some point, but by then the paralysis is already severe. Over time scar tissue forms, blocking signals, leaving the patient paralyzed below the injury — in the arms and legs if it’s in the neck, or just the legs if in the lower back.”
Engineering a human spinal cord in the lab
“The goal is to build a small piece of spinal cord that behaves like the real thing. We can remove the scar tissue, implant the engineered tissue in its place and eventually fuse the new piece with the existing cord above and below the injury. Think of it as inserting a conductor between two cut cable ends, restoring communication,” he said.
The challenge is rejection by the body’s immune system. “When tissue comes from another source, the body may attack it. Even if the implant is good, the immune system creates a fibrotic layer around it that blocks the electrical signal,” he explained. “That happens with many implants — breast implants, pacemakers. But here, where the tissue must conduct electricity, insulation ruins the function.”
To overcome this, the team developed a personalized solution. “We take blood cells from the patient. They’re not neurons, but using a Nobel Prize–winning technology from 2012, we reprogram them into stem cells with the ability to become any cell in the body,” Dvir said.
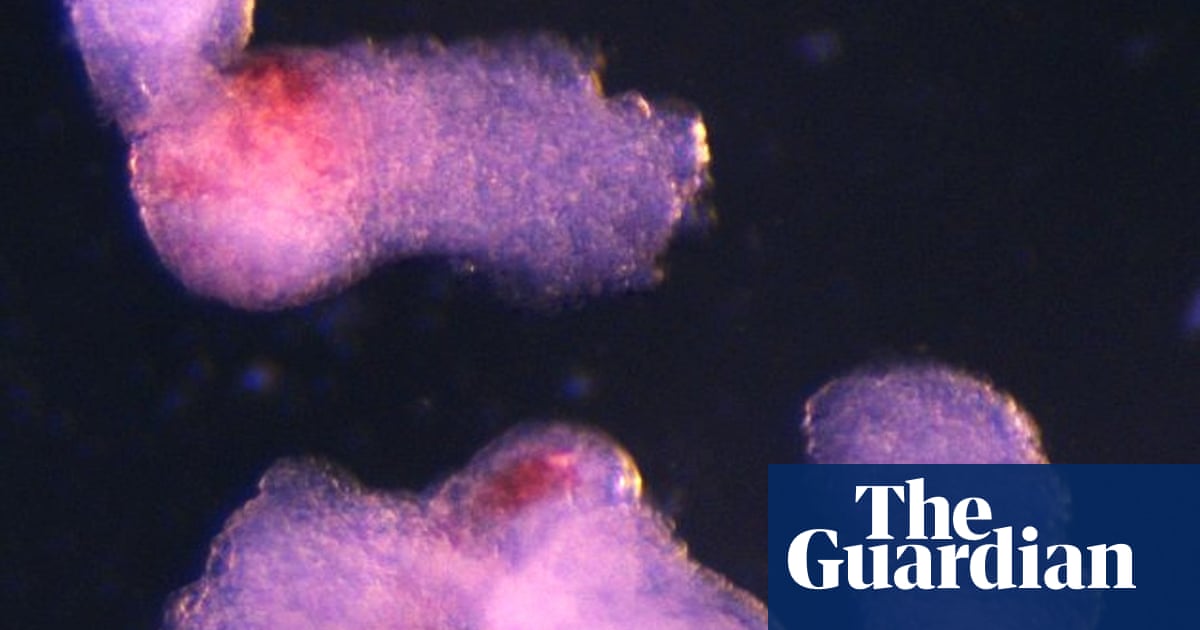
Next comes tissue construction. “Cells alone aren’t enough — if we inject neurons, they’ll die. They need to be organized into tissue,” he said. The researchers harvest fat tissue from the patient, extract collagens and sugars, and use them to create a gel. “This gel is also personalized, just like the cells. We place the reprogrammed stem cells in it and mimic embryonic spinal cord development.”
3 View gallery


Prof. Tal Dvir says the first recipient of the new technology will be Israeli
(Photo: Matricelf)
The result is a full 3D implant. “After a month, we have a three-dimensional tissue full of motor neurons transmitting electrical signals,” he said. “We then implant it at the site of the injury.”
From animals to humans
Now comes the human trial. “We submitted our results to Israel’s Health Ministry. Six months ago, we received initial approval for compassionate-use trials in eight patients. Of course, the first patient will be Israeli,” Dvir said. “The technology was developed here, and I trust Israeli surgeons to perform it best. We already have approval to begin drawing blood as soon as the first patient is chosen and cleared.”
The treatment is initially limited to relatively recent injuries, less than a year old. “We won’t start with the most severe cases,” Dvir said. “But once we prove it works, the possibilities are open. We’ll then define criteria like age and injury location, but ultimately, I believe this will help all patients with paralysis.”
Alongside Dvir, key figures driving the project include Matricelf CEO Gil Hakim; Co-founder, Deputy CEO and President Dr. Alon Sinai and Vice President R&D Dr. Tamar Harel Adar with her team. “They got us to approvals so quickly — it’s amazing,” Dvir said.