Today is World Thrombosis Day. On this day, someone to remember is Rudolf Virchow [1821-1902], a German physician, pathologist and politician, referred by his colleagues as the “Pope of Medicine.” His famous postulate: that for blood to clot, three factors are needed — stagnation, injury to vessel wall and abnormalities in clotting mechanism — remains unchallenged to this day.

Understanding clotting
Clotting is important because it can be symptomless and yet cause sudden death. Clotting in the veins of the legs – acute deep vein thrombosis in medical terms – which sometimes floats its way to the lungs (pulmonary embolism) is the most preventable cause of hospital deaths and a source of substantial long-term morbidity. About 120 of every 1 lakh persons are affected by this malady.
The most common causes of thrombosis are prolonged immobility due to trauma, spinal cord injuries resulting in paralysis, major neurosurgery, pelvic surgery or orthopaedic surgery, especially hip and knee replacement surgeries, and extended stays in intensive medical care units. Some diseases such as cancers and certain viral infections also interfere with the coagulation cascade and can promote a clot. The common viral infection H1N1, causes a 23.3-fold higher incidence of pulmonary embolisms and 19.9-fold higher incidence of deep vein thrombosis. A number of patients recovering from chicken pox, a viral disease, also present with clots in their legs. Drugs including oral contraceptives, hormone replacement therapies and some cancer drugs also promote clots in the veins. Catheters left in the central veins for a prolonged period also promote clots. Physiological stagnation and clotting can also occur during pregnancy and the early postpartum period. Smoking is a definite cause for atherosclerosis as well.
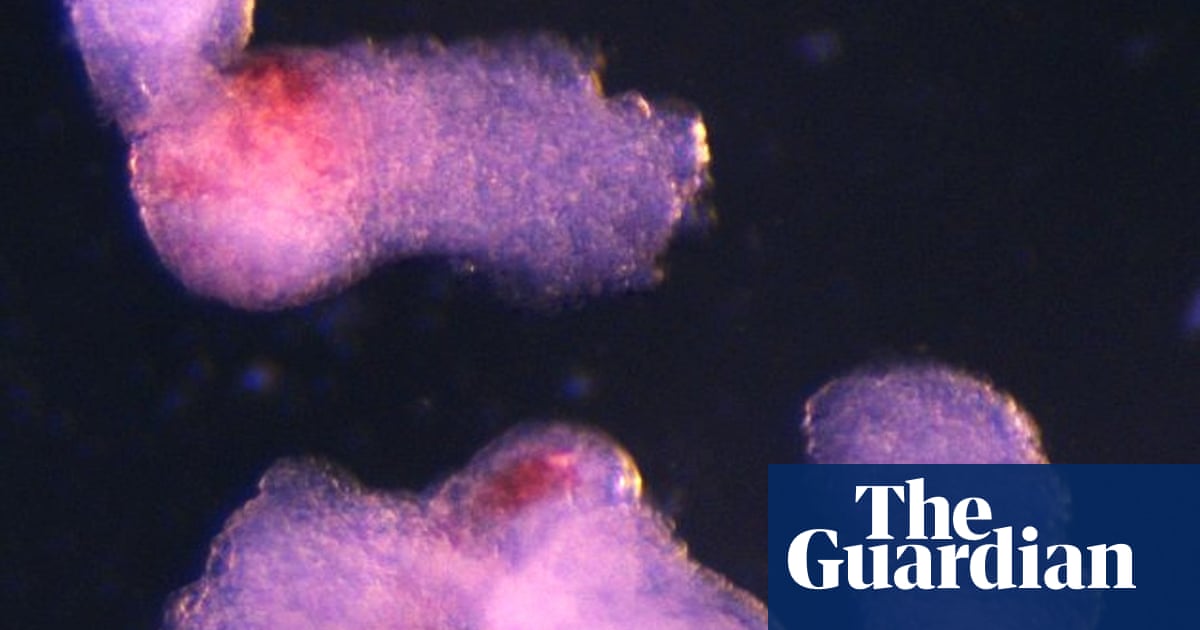
How clotting occurs
When a person is immobile, blood stagnates in the veins of the legs, the soleal veins, and promotes clot formation in the valves present in those veins. This is worsened by inactivity of the calf muscles. Calf muscles act as a pump, pushing the blood upwards to the heart. They are considered the peripheral heart or second heart. Any form of mobility such as walking, climbing stairs, running or cycling pumps venous blood from the lower limbs towards the heart, and hence should be vigorously encouraged in normal populations as well as those convalescing from various diseases or recovering from major surgeries.
There are many reasons why clots in the legs are bad: first such a clot can detach itself from the walls of the leg veins, move all the way to the lungs, choke them and cause sudden death. Most often this is so sudden that there is no time to even plan a definite treatment to save these patients. Second, these clots can recanalise but also cause narrowing of the blood vessels of the lung. They may not end in sudden death but can cause severe breathlessness even with minimal exertion leading to pulmonary hypertension. And lastly, the leg veins and the valves where the clots form, can be permanently damaged. They lose their capacity to pump blood upwards to the heart, leading to constant pooling of blood in these veins. The ‘second heart’ therefore is damaged forever. Rarely, massive thrombosis in leg veins can result in gangrene of the limb and even death. Hence prevention is the best primary choice, and in cases where a clot has occurred, very early diagnosis and prompt treatment to prevent the growth and migration of the clots and prevent vein valve damage is essential.

Prevention and treatment
How does one prevent these dreadful clots? While prevention of vessel wall injury or inherent defects in the clotting mechanism may not be possible, stagnation can certainly be avoided through the aggressive promotion of physical exercises and adequate hydration to keep the blood optimally diluted.
Any exercise, starting from the simple tiptoe exercise to running, helps prevent stagnation. Prolonged immobility in any long-distance journey predisposes an individual to venous stagnation. Walking inside an aircraft especially in long-haul flights is a proven way to prevent clots, as is good hydration. Avoid alcohol on long flights because inebriation adds to immobility. If it is a car journey, break the journey every three or four hours get out and walk around a little, and stay hydrated.
If a surgery is planned, especially a knee or hip replacement, a discussion should be had with the surgeon about anti-clot protocols and early ambulation. Similarly, for those who are bed ridden for a long time, compression stockings and intermittent pneumatic compression devices are available. A doctor will be able to guide patients as to which one would be appropriate. In some instances, filters placed in the great vein, inferior vena cava, can prevent the migration of clots from the legs to the heart. There are very specific indications for such procedures and the treating doctor would be the best person to decide that.
Once a clot in the leg veins is detected, prompt treatment is needed. In select cases, clot dissolving chemicals commonly known as clot busters, can prevent damage to the veins and vein valves. In severe cases, surgical removal of the clots from the lower limbs or from the pulmonary blood vessels may be lifesaving. A specialist is best placed to decide on treatment, depending on the case.

Move your limbs
As with all diseases and disorders, prevention is the best strategy. Stay hydrated, stay mobile and those who have inherent abnormalities in clotting factors should continue clot preventing medications unless specifically stopped by the treating doctor. Smoking and consumption of alcohol promote arterial thrombosis and are best avoided.
(Dr. J. Amalorpavanathan is director (retired), Institute of Vascular Surgery, Madras Medical College. amalorpavanathanjoseph@gmail.com)
Published – October 13, 2025 02:01 pm IST
Source link